From January 2012 to September of 2016, there was a minimally formal quality improvement and assessment program (QAPI) within the Mayo Clinic Transplant Center in Phoenix, Arizona. Attempts had been made to grow the program, but success was limited, as assessed by broader metrics of process improvement projects, engagement by the organization, and standardization of metrics, meeting cadence, and outcomes reporting. Improving the structure and formalization of the QAPI program can improve the transplant process effectively and efficiently to enhance the patient experience and improve volumes and outcomes.
Aim Statement
We aimed to create a formalized QAPI program for the Transplant Center with a set of standardized metrics and outcomes reporting, engagement in quality improvement from the organization, and process improvement projects by December 31, 2019.
Define and Measure
The Define, Measure, Analyze, Improve, Control (DMAIC) process improvement methodology was used. In the Define and Measure phases, an overall assessment of the Transplant Center was performed. First, the scope of the program was determined through an assessment of strategic vision, mission and objectives as well as a formal gemba walk of high-level processes. This also helped define customer requirements, which led to gathering baseline data on those requirements.
Vision: Mayo Clinic Transplant Center in Phoenix will be the most trusted partner for health care and be recognized as a premier patient-centered academic transplant center.
Mission: Mayo Clinic Transplant Center in Phoenix will inspire hope and provide the best care to every patient through integrated clinical practice, education and research.
Strategic Objectives:
◉ Increase preference for Mayo Clinic Transplant Center in Arizona among physicians and the public.
◉ Grow transplant volumes, particularly living donor programs.
◉ Increase customer satisfaction: patients, referring physicians and third-party payers.
◉ Enhance financial performance.
◉ Improve patient access and navigation.
◉ Enhance patient safety.
◉ Sustain high quality in each organ program.
◉ Recruit, train and retain the best staff.
◉ Develop research and education programs.
◉ Promote organ donation in the community.
◉ Develop and mature existing partnerships and collaborations.
The team developed an understanding of key transplant metrics as well as established outcomes reporting, a QAPI meeting schedule and a formal QAPI plan.
Figure 1: Transplant Process
Additionally, an assessment of engagement in quality was made. At the time of this assessment, the key measures for the overall QAPI program were engagement (defined as number of people trained in QI; baseline: 2 persons), QI projects executed (baseline: 1) and standardization of metrics and outcomes reporting (baseline: 0).
Analyze
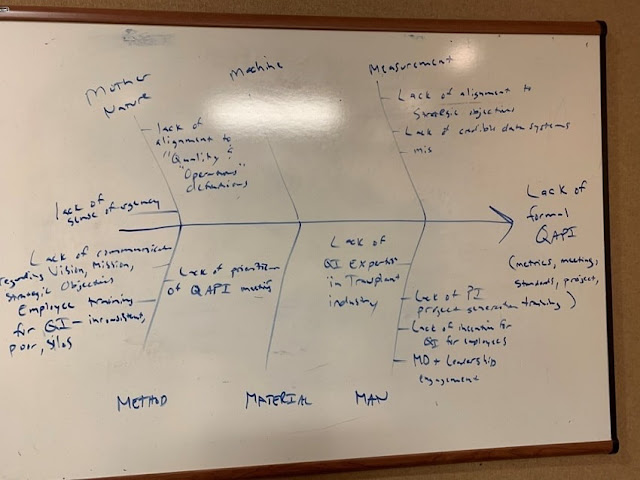
In the Analyze phase, high-level process maps and root cause analysis were used to identify key factors contributing to the gaps in obtaining and reporting the metrics, meeting cadence, standardization of reporting and presentations, and project generation and documentation of QI activities.
Figure 2: Root Cause Analysis Exercise
Root causes found included, but were not limited to:
◉ Lack of sense of urgency for QI
◉ Physician and leadership engagement
◉ Lack of communication regarding the vision, mission, strategy and objectives
◉ Employee training and awareness of QI
◉ Lack of formalized schedule and prioritization for QAPI meetings
◉ Lack of prioritization and alignment of strategic objectives and QI
◉ Lack of accountability on action plans – minor improvements to the practice
◉ Lack of formal QI project generation and documentation
◉ Misalignment of operations and quality definitions
◉ Lack of QI expertise resources within transplant
Improve
In the Improve phase, interventions began to be implemented around standardizing the scheduling of QAPI meetings, the adverse event process, data reporting, data automation, metrics/outcomes needed for presentations, and formalized QI training and project generation. This was created over a phased approach to aid in change management for the organization (see Figure 3).
Figure 3: Phased Approach
One of the first steps was clarifying the sense of urgency for QI, engagement and communication. QAPI meetings were reinvigorated by leadership, then formalized and standardized in terms of timing. A template presentation for the QAPI meetings as well as a holistic dynamic dashboard were developed from multiple sheets (N=15, 280 entry fields) to simplify the key metrics that were required and needed to understand the practice as a whole. Automation of those key metrics was then incorporated into the presentation packages to aid in efficiency and effectiveness of the use of the data for decision-making as well as a final website using an analytic software called Tableau (see Figures 4 and 5).
Figure 4: Data and Presentation Flow
Figure 5: Simple Dynamic Dashboard
During the phased approach, an 80/20 strategy was deployed for projects, engagement and confidence builders to the organization. Early in the phases, 80 percent of projects would be small in scope with a high variation of metric, while 20 percent would be large in scope with potentially inconsistent or no data available. As the organization progressed in projects, engagement and confidence, this relationship would reverse: 80 percent focus on large-scope projects and 20 percent on small confidence-builder projects.
Training
In addition, a transplant-specific Silver Quality Essentials course (a diluted version of an industry-standard Yellow Belt training) was integrated with a standardized Mayo course from Quality Academy, featuring tailored examples to transplant data, time and resources. This training allowed for not only QI awareness and education but change management to garner the confidence of the organization – both of QI itself and to drive more project generation.
Started as Flow-Based System
Prior to formal training execution, the final aspects of the business review were performed to help scope projects. The Transplant Center lacked a formal prioritization method but the system was largely a queue/flow-based system. Standard Lean and operations management principles can be quickly applied to harvest confidence-builder projects in this type of setting. The team’s first exercise involved using Little’s Law to articulate the flow of the system and where bottlenecks may lie. From there, Six Sigma tools were used to address variation reduction. Both of these methods led to the unique targeted approach for this culture and situation to net the highest benefit.
Transplant = Flow system
◉ Transplant “factory” physics and math applied
◉ Little’s Law/theory of constraints – first set of assessment tools
◉ Six Sigma (defect reduction) – second set of assessment tools
Little’s Law Assessment (First Exercise)
WIP = R * T
Where,
WIP = waitlist patients (avg/year, active)
R = throughput rate (transplants/year)
T = lead time (referral to transplant [TX], avg 2020)
In this assessment, WIP and R were known and reported publicly. Standardized definitions for all transplant centers were available and were used as a base start to assess the organization.
For the assessment, T = WIP/R, which would facilitate what the organization should be operating at, defined by the Little’s Law proof.
| Actual Lead Time for Three Organs | |||
| Kidney | Heart | Liver | |
| WIP | 521 days | 38 days | 113 days |
| R | 327 days | 50 days | 127 days |
| T | 1.59 years | 0.76 years | 0.88 years |
Source: SRTR, UNOS, Mayo Clinic EMR
From here, we know what the actual lead time should be for three organs: Kidney = 1.59 years, Heart = 0.76 years and Liver = 0.88 years. At the same time, a new internal tool was being developed (called EDITLIFE) that could give us the current-state lead times as they were happening internally. This current-state assessment gave us:
| Current-State Lead Time for Three Organs | |||
| Kidney | Heart | Liver | |
| WIP | 521 days | 38 days | 113 days |
| R | 327 days | 50 days | 127 days |
| T | 1.75 years | 1.4 years | 1.21 years |
The Kidney, Heart and Liver programs average lead times (referral to transplant) were 638, 511 and 441 days (1.75 years, 1.4 years and 1.21 years, respectively). Notably, the Heart program was operating at two times the lead time that it should be. Knowing that many of the processes have the same set of bottlenecks – such as a holistic meeting of review of patients called “Selection Conference” and a slew of insurance authorizations – now we moved to our Six Sigma and variation reduction tools (second exercise) to precisely target our confidence-builder projects.
The analysis of variance (ANOVA) test showcased that while there was a statistically significant difference between the groups (p-value = 0.0067), the Kidney program had the majority of the variation followed by the Heart program, as shown in the Tukey-Kramer Connecting Letters report. (See Figure 4.)
Figure 6: Six Sigma Work
What is critical here is the ANOVA showed us that our biggest win would come from the Kidney program (more samples = 248 kidney transplants vs 40 for heart transplants during the analysis period), not from the Heart program as one might expect. We now knew how to guide the organization into its first set of projects. When the Kidney team members came to training and we asked, “What is your biggest problem in the Kidney Transplant Center?” they replied, “Speed to getting a transplant!” That translated to lead time.
Our first project, thus, was a Kidney transplant “selection to listing” lead time project that lead to massive improvements for the organization. We worked to build the relationship, confidence and rapport with the teams.
Had we not chosen a guaranteed “winner” project to start, in the absence of a formal strategic prioritization of processes like business process management (BPM), our success story may have never occurred.
From September 2016 to the end of December 2018:
◉ 68 individuals were trained in QI
◉ 100 QI projects (10 DMAIC, 12 PDSA and 78 action plans) were completed
◉ A formal standardized dashboard, standardized presentation QAPI package, consistent QAPI Subcommittee meeting schedule and formalized communication foundation for leadership engagement and process flow were enabled
QI engagement (as measured by training) and QI projects and outcomes summary graphs are featured in Figures 7 and 8 and Table 2, respectively. Finally, our counterbalance of patient satisfaction stayed the same, which we consider a success; we were able to move patients faster through our system without adversely affecting their satisfaction (see Figure 9).
In total, the cumulative return on investment (ROI) of this operational excellence deployment model was $28.8M. Of this, $11.2M were from operations cost reduction and efficiency gains (net present value [NPV] method used) and $17.6M were from revenue increase models, attributed to one project (Living Kidney Donor Transplant Improvement) with standard revenue recognition models used for this measure.
Figure 7: Engagement via Training
Figure 8: QI Projects
Table 2: Detailed Outcome Summaries (Click to Enlarge)
Table 3: Simplified Outcome Summaries
| Results | Benefits to Patient |
| Reduced immunosuppression documentation errors from 3 errors/month to 1 error/month | Induction errors documentation – pharmacy, nursing and anesthesia collaboration to reduce the documentation errors of drug dosages given to patients |
| · Reduced non-value-added calls to transplant call center from 1,420/week to 1,100/week · Moved flow of non-value-added calls to message center |
Effective call center triage – reducing the number of non-value-added calls made to the transplant call center to effectively manage appropriate calls |
|
· Reduced selection to listing time frame from 73 days to 18 days |
Selection to listing process change – historically, patients were brought to selection conference without all evaluations completed for discussion |
| Improved ABO verification compliance from 85% to 97% across all organs | Opportunity to reduce ABO verification errors with heart and liver, first, followed by kidney – all solid organ transplant programs |
| Improved process for liver patients getting feeding tube placement, logistics and financing | Optimizing the flow for feeding tube process for liver patients |
| · Reduced the time from 289 min/request to .46 min/request · Increased the effectiveness of knowledge gained from 58% to 100% |
Reducing the time and increasing the effectiveness of the transplant scheduling team with regards to scheduling processes |
| Increased awareness on transplant quality data knowledge from 81% to 100% | Metrics awareness project for 3W nursing team (CMS item) |
|
· Reduced waitlist time for kidney patients from 633 days to 458 days |
3 DMAIC projects in 1 – UNOS collaboration for high-risk kidney donation |
| Reduced referral-to-listing throughput time from 72 days to 46 days | Reducing the time from referral to listing for heart program candidates |
| · Reduced referral data accuracy rate from 89% defective to 0% defective · Reduced 77 hours of FTE wasted time on error connections annually |
Referral data accuracy for all organ groups |
| · Reduced recipient evaluation to transplant from 289 days to 126 days · Reduced donor referral to donation from 163 days to 147 days |
Reducing time from referral to transplant for both recipients and donors |
Figure 9: Counterbalance – Patient Satisfaction









0 comments:
Post a Comment